In 2023, the media have been brimming with content about AI and ideas on how it will transform medicine. The entry of ChatGPT almost exactly a year ago put AI front and center for everybody. The change has been happening so fast that many of us feel poorly prepared to keep up. The approach to AI in healthcare spans from doing nothing to developing own solutions or adopting marketed technologies. Many hospitals and clinics are still not ready for the adoption of even well-tested technologies.
Limitations and Challenges of AI/ML in Medicine
It is tempting to ask ChatGPT the question about AI adoption in medicine, but, likely, the answer will not be completely right.
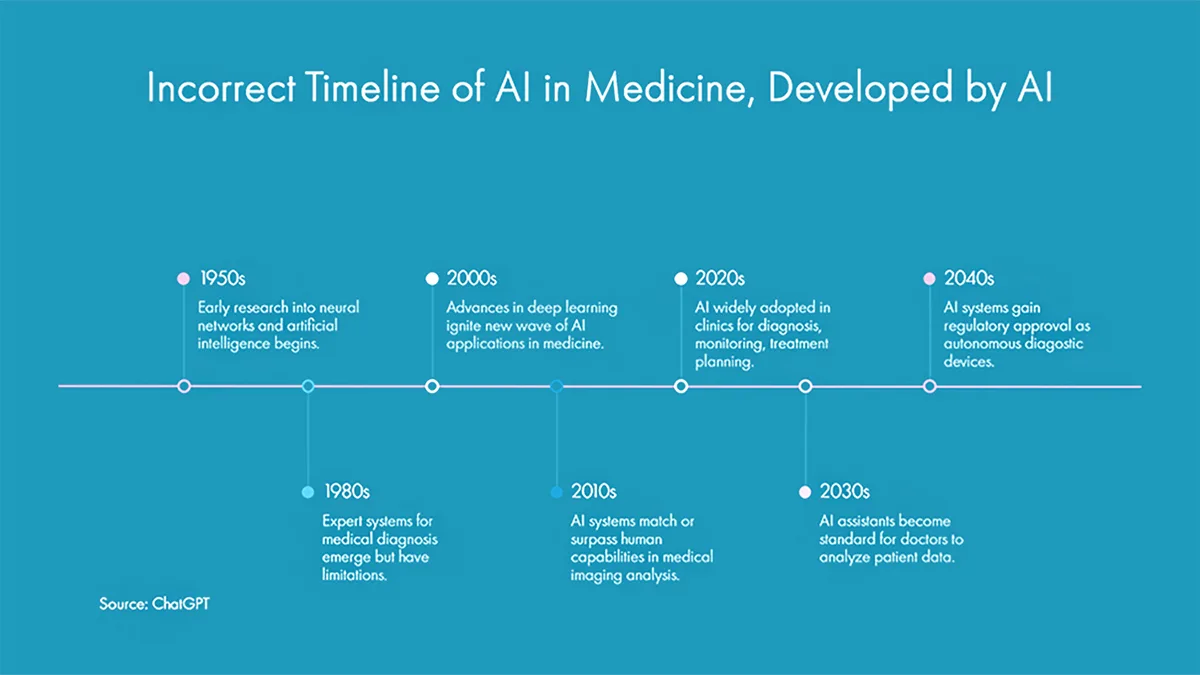
This is because ChatGPT uses information from the internet and has no independent knowledge of what information is right and what isn’t. In this example, it is not true that medical imaging surpassed humans in 2010s or that in 2020s AI is widely adopted in clinics. Imagining has become very precise and sometimes surpassing expert radiologists only recently, and even now AI solutions are not broadly adopted in healthcare.
Any AI is as good as data on which it was trained and has access, so medically useful AI solutions must be trained on proper medical data. This is the main challenge in developing AI solutions in medicine, because of a vast proportion of unstructured data (data that cannot be easily put in tables, such as a patient medical history), and multimodal data (e.g., text, pictures, and sounds). Multimodal AI for medical practice is currently being tested and may be released within the next months. In addition, the generalizability of AI/ML solutions across different populations is limited, for example, an AI algorithm trained in a big urban academic center may not perform as well in hospital located in a rural, lower resource environment due to differences in treated populations.
Several other challenges should be considered when developing AI/ML in medicine:
- Limited knowledge among hospital administrators and clinicians regarding AI/ML solutions, leads either to total rejection or lengthy review process before implementation. It is not to say that review is not necessary, but that many hospitals do not have the process to quickly assess new technologies.
- Healthcare data is highly sensitive, requiring robust privacy measures that can impede accessing data for developing AI.
- Algorithmic biases stemming from biases in a training dataset may lead to serious clinical mistakes, as observed in a few cases when AI treated patients of color differently from Caucasians.
- The “black box” phenomenon, meaning a lack of transparency in how the algorithm works and therefore inability to explain how it reaches its conclusions.
- Clinicians are rarely involved in the development of AI algorithms, what sometimes leads to solutions that are not clinically relevant or don’t match existing clinical workflows. Improved collaboration between various stakeholders is necessary to develop clinically useful AI/ML, but it is continuously difficult to form research teams with combined clinical, subspecialty, engineering, and computer science expertise.
Addressing these challenges is necessary for the evolution of AI/ML technology and realizing its potential in medicine.
Current AI/ML Use in Medicine
Despite challenges, there are already several successful uses of AI/ML in medicine, especially in diagnostics, drug discovery, clinical decision support and personalized medicine.
- AI can analyze medical images and detect abnormalities earlier and more accurately than doctors. It can enhance the analysis of medical images, such as X-rays, CT scans, and MRIs, to improve diagnostic accuracy and reduce the workload on radiologists.
- AI can speed up drug discovery by screening millions of chemical compounds and analyzing data to find promising drug candidates. AI automates the identification of potential drug candidates and predicts their effectiveness. Also, AI can assist in various aspects of medical research, from analyzing large datasets to identifying potential drug targets and repurposing existing drugs for new uses.
- AI can analyze data from wearable devices and other remote monitoring tools to track patient health and provide real-time feedback to healthcare providers.
- AI can provide treatment recommendations based on patient data and medical knowledge to assist doctors in making clinical decisions.
- AI can analyze patient genomics, metabolomics, lifestyle, and medical history to provide personalized prevention and treatment plans.
- AI-driven robotic systems, such as the Da Vinci, can assist surgeons in performing complex procedures with greater precision and control.
- AI can streamline administrative tasks, such as appointment scheduling, medical record management, and patient follow-ups, reducing the burden on healthcare professionals.
- AI can analyze large datasets to identify trends and patterns in population health, helping to inform public health policies and interventions.
The growth of AI algorithms in medicine leads to very enthusiastic business forecasts, with a prediction of 30% CAGR (Compound Annual Growth Rate) for the next ten years.
Common Myths
With the fast growth of AI, many fear what it means for them and the practice of medicine. I am convinced that AI/ML will change the ways we work, but I don’t subscribe to catastrophic views. Common myths include:
AI will replace doctors. AI augments and assists doctors but is not able to think critically and has no intuition, AI may replace simpler, more common tasks and may recommend diagnosis and treatment. By eliminating human biases, it will help doctors to do better. Doctors who use AI will eventually replace doctors who don’t.
However, AI may replace some administrative roles due to the ability to generate intake and discharge documents, schedule appointments and quickly analyze data. It’s also very likely that other jobs will be improved by removing the administrative burden.
AI must be flawless. Doctors make mistakes, but we expect AI/ML to be flawless. It is not possible and should not be required as long as AI adds value over current standards of care. However, we also should be aware of the “automation bias,” meaning the belief that a digital solution provides better results than a human being.
AI is universally applicable. Due to differences in patient populations between healthcare systems, the AI solution developed in one location may not be fully applicable in another hospital or clinic. Differences in population translate into very different training data sets and therefore different algorithms. An algorithm may have to be retrained or developed anew for a new setting.
The Future
While AI has great potential in medicine, we need realistic expectations about its current and future abilities and limitations. I am positive that while addressing challenges, we will continue to develop and implement new solutions for the benefit of patients, clinicians, and the healthcare system.
Also Read: The AI-powered Future: Will We Live Healthier, Longer Lives?
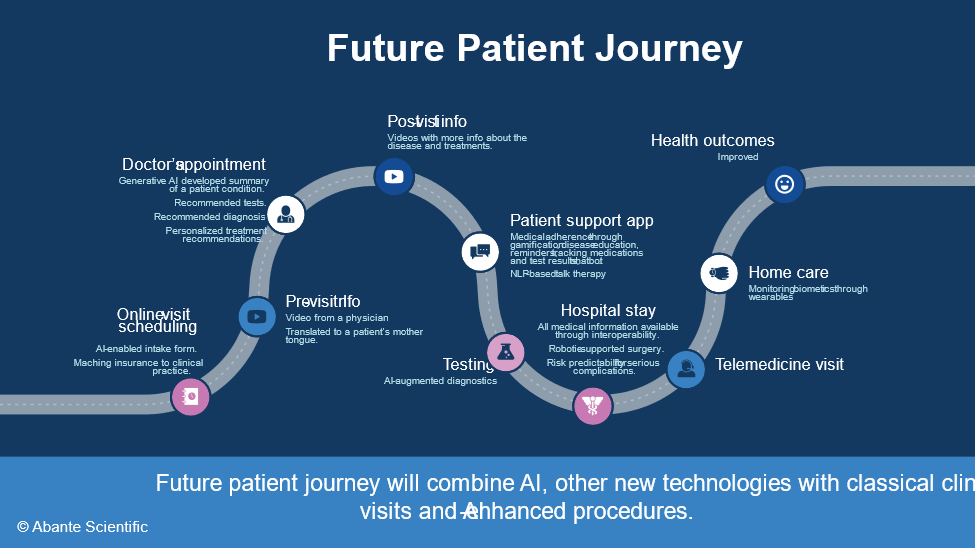
My hope is that we will enhance patient experience and outcomes in the future, by smoothly incorporating new technologies into the existing physician workflows and patient journeys. The slide below shows how it can be done, with technologies that are already available or in development.